PBMs and such (breaking it down for the average human)
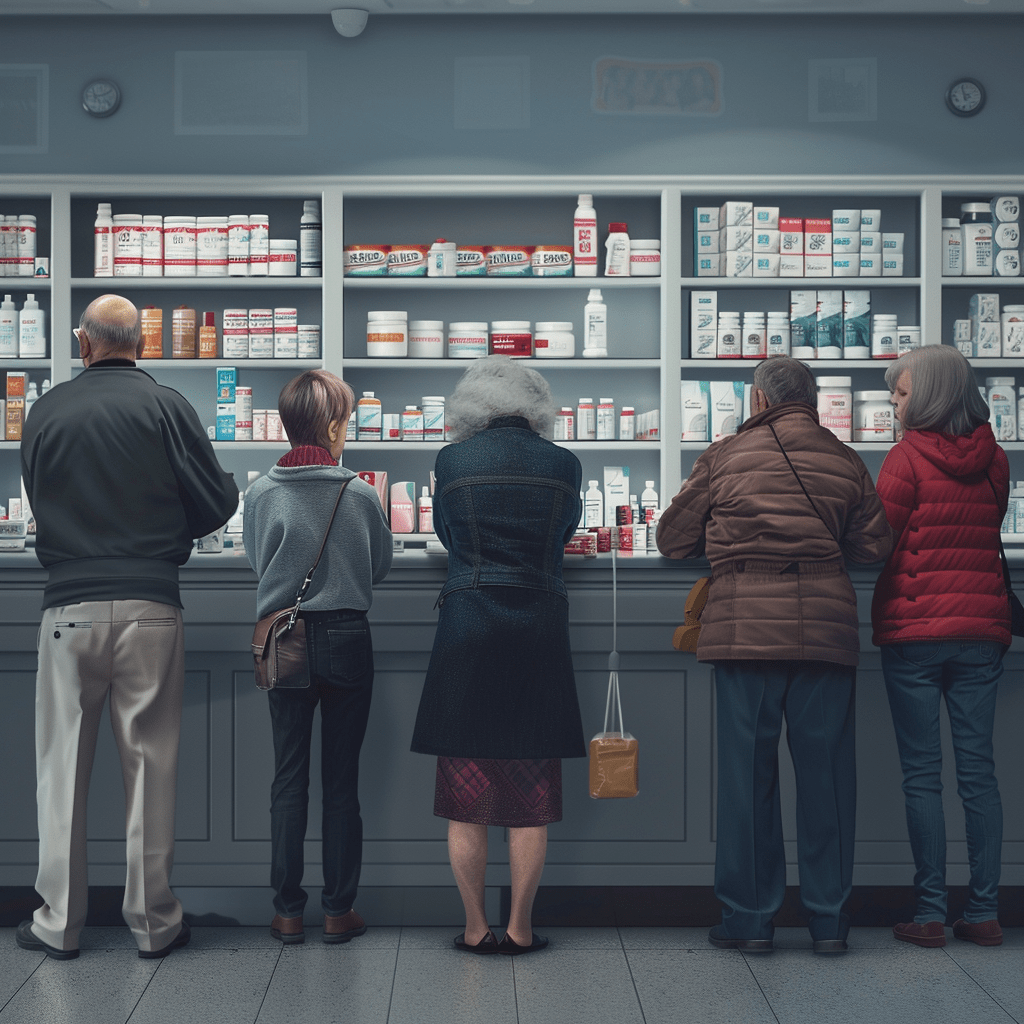
As patients living with autoimmune diseases, we rely on our local pharmacy and pharmacists to access the doctor-prescribed medications we need as well as to advise us on a range of health and pharmaceutical
concerns. However, so-called Pharmacy Benefit Managers (PBMs)—the healthcare middlemen that seem to control prescription drug access—are making life harder for both patients and independent pharmacies.
This is a problem that Congress needs to fix. Patients already deal with enough restrictions and limitations imposed by PBM policies, which help these insurer-owned groups to boost profits ever-higher. For patients, these unfair practices can delay access to care or even force them to go without their medications until patients can “prove” they need them.
Meanwhile, PBMs can also restrict patients from using PBM-affiliated pharmacies—usually to the larger chains—if they want to access their prescriptions. Look, we don’t want to go out of our way to receive less personalized pharmaceutical care than what we enjoy about our local, independent pharmacy so PBMs can scoop up even more profits. We also don’t want to see the pharmacy I’ve been going to for 10+ years go out of business because of these unnecessarily restrictive, anti-competitive policies.
Congress should pass PBM reform like the Delinking Revenue from Unfair Gouging (DRUG) Act to rein in PBM practices and help protect patient access and the independent pharmacies that are part of our communities.
William Miller and Penny Lane
